Millimeter-wave/microwave ablation (essentially, heating by use of millimeter-wave and microwave electromagnetic radiation) has been proposed as a means of treating atherosclerotic lesions. Computational simulations have shown that by controlling and customizing temperature profiles in millimeter-wave/ microwave ablation, it should be possible to (1) treat atherosclerosis or coronary thrombosis without (2) incurring the distensions and injuries to arterial walls and epithelial walls that are common to current invasive treatments, while (3) possibly reducing post-treatment inflammation and even restenosis. Although millimeter-wave/microwave ablation has yet to be proved in tests on live animals, it offers the potential to signifi- cantly advance the state of the art. Indeed, after further testing, millimeterwave/ microwave ablation might be used by cardiologists during balloon angioplasty replacement procedures (PTCAs) or coronary catheterizations. Because it is expected to be safer and more effective than traditional methods, millimeterwave/ microwave ablation could soon supplement or even supplant today’s treatment choices.
In millimeter-wave/microwave ablation, advantageous temperature profiles would be obtained by controlling the power delivered, pulse duration, and frequency. For best results, the profile would be chosen so that the maximum temperature is delivered at the center of an atherosclerotic lesion and the temperature would decrease, uniformly in all directions, with distance from the center. The heating would favorably modify lipid-rich lesions that contain the inflammatory cellular infiltrates that are prone to rupture, and the rupture of which causes thrombotic artery occlusions (heart attacks).
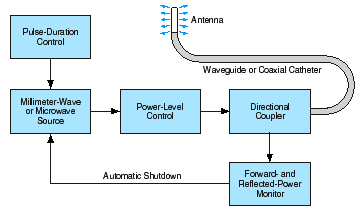
The major components of an apparatus for millimeter-wave/microwave ablation apparatus (see figure) would include a millimeter-wave/microwave source, a catheter/transmission line, and an antenna at the distal end of the catheter. The source would generate millimeterwave or microwave power at a controlled level up to 10 W, with a pulse duration between 0.1 and 10 s controlled to within 2 percent. A chosen frequency between 2 and 300 GHz could be used; a separate source would probably be needed for each frequency. The catheter/transmission line would deliver the power to the antenna.
The antenna would focus the radiated beam so that most of the millimeter-wave or microwave energy would be deposited within the targeted atherosclerotic lesion. Because of the rapid decay of the electromagnetic wave, little energy would pass into, or beyond, the adventitia. By suitable choice of the power delivered, pulse duration, frequency, and antenna design (which affects the width of the radiated beam), the temperature profile could be customized to the size, shape, and type of lesion being treated. By controlling temperature, one could limit (1) the damage to the endothelial layers and (2) the risk of overheating nondiseased tissue and proximal blood. For safety, the control system of the apparatus would provide automatic shutoff in the event of an inappropriate power level, excessive reflected power, unsuitable pulse duration, or heating beyond prescribed limits.
This work was done by Patrick Fink and G. D. Arndt of Johnson Space Center; J. R. Carl and Reginald Beer of Lockheed Martin; George Raffoul of Hernandez Engineering, Inc.; and Philip Henry and Antonio Pacifico. For further information, access the Technical Support Package (TSP) free on-line at www.nasatech.com/tsp under the Electronic Components and Systems category. This invention has been patented by NASA (U.S. Patent No. 6,047,216). Inquiries concerning nonexclusive or exclusive license for its commercial development should be addressed to the Patent Counsel, Johnson Space Center, (281) 483-0837. Refer to MSC-22724.