Nilesh Salvi and Jinglu Tan
University of Missouri
Columbia, MO
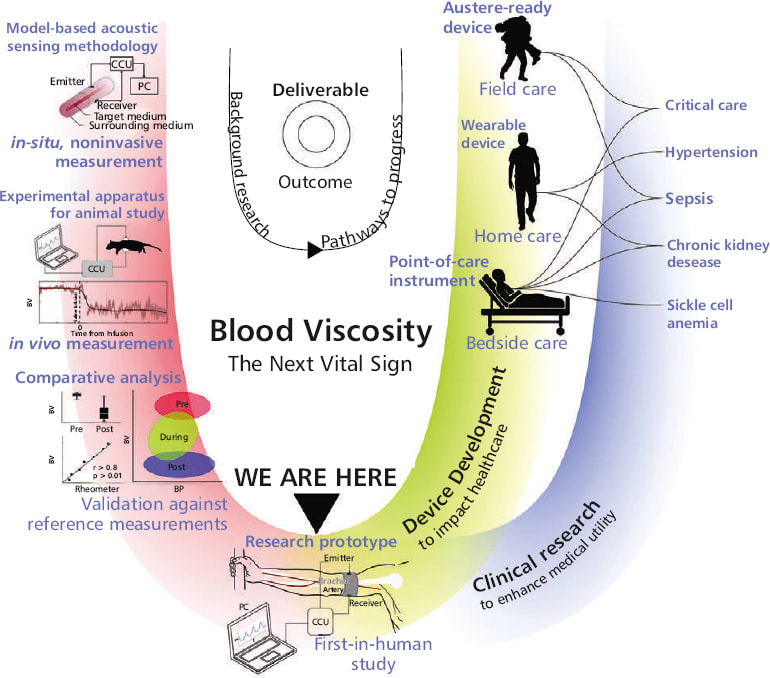
The first real-time, wearable blood viscosity (BV) monitoring device fills a long-standing void in trauma, burn, and sepsis care by delivering continuous, noninvasive insights into the body’s fluid and vascular dynamics.
“The concept began with our in-situ viscosity measurement work on industrial fluids,” said Nilesh Salvi of University of Missouri. “During NSF-supported customer interviews, we identified blood viscosity as a long-overlooked factor in medicine, despite its central role in circulation and oxygen delivery. Poiseuille’s law made it clear that viscosity matters as much as pressure, yet clinical practice lacked tools. Existing lab methods were slow, invasive, and disconnected from physiology, and their shortcomings were mistaken for limitations of viscosity.”

These insights, combined with the high-reward potential for understanding disease and advancing healthcare, inspired the team to develop an ultrasound-based system capable of measuring viscosity in vivo and in real time.
Unlike traditional vitals, BV reflects the blood’s resistance to flow — capturing subtle, early physiologic shifts caused by dehydration, systemic inflammation, coagulation changes, and vascular leakage. These are the earliest precursors to life-threatening conditions like sepsis or hemorrhagic shock. “Our technology empowers clinicians and medics — whether at the bedside or in remote, resource-limited environments—to respond before deterioration becomes irreversible,” said Salvi.
The platform is built on a patented ultrasound-based sensing method, originally developed and validated in animal models, with tight correlation to gold-standard viscometers. It uses compact, rugged off-the-shelf components and is engineered for scalability and low-cost production.
Integrating cuffless blood pressure, the system creates a hemodynamic dashboard: dynamic BV–BP patterns reveal whether resuscitation is on track, failing, or overshooting. This combination unlocks unprecedented diagnostic resolution, enabling smarter fluid management, triage precision, and downstream therapeutic decisions. Early validation in rats shows distinctive viscosity trends, even when BP remains unchanged, with cluster analysis revealing patterns unique to BV that BP alone cannot detect — highlighting the untapped value of BV as a vital parameter. The software-driven architecture accelerates regulatory readiness and enables integration with next-gen autonomous resuscitation systems.
This device redefines physiologic monitoring — it introduces a novel lens into the body’s dynamic response to trauma and disease by uncovering real-time blood flow resistance patterns and volume status, enriching clinical understanding of vascular health and systemic stress. For sepsis, the device detects early-stage coagulopathy and fluid shifts before traditional signs emerge.
In the long-term, this technology could transform drug development for cardiovascular disease and metabolic syndrome by establishing viscosity as a biomarker of vascular health and drug response. For the military, it enhances survivability in the “golden hour” post-injury; for civilians, it introduces a new frontier in personalized critical care.
“We are pursuing a dual-track strategy. The primary path is FDA approval of the clinical-grade system, estimated at 4–6 years. In parallel, we are developing a consumer-oriented wearable with a 2–3 years’ timeline for wellness, athletic recovery, and research markets,” said Salvi.
“Our initial entry point will be clinical research laboratories. From there, we plan to expand into nonclinical wearables as an early market, while critical care, sports medicine, chronic disease, and military medicine remain later-stage markets dependent on FDA approval. This phased approach balances nearterm revenue opportunities with the long-term value of regulatory approval,” he added.
The team has de-risked the core technology through NSF-funded prototypes, patented methods, and strong preclinical data. The commercial roadmap targets emergency care, remote monitoring, and digital health markets. With its unique ability to generate previously invisible physiological insights, blood viscosity is poised to become the next vital sign — redefining standards of care, unlocking new therapeutic strategies, and saving lives across settings.
For more information, visit here .