Undergoing treatment for a physical injury or condition can be a long and frustrating experience. Broken bones, sprains, torn muscles or ligaments, as well as painful conditions that have developed over time, like carpal tunnel syndrome, need customized treatments. Physical therapists could benefit from a measurement-based approach to retraining patients for proper movement and mechanics.

Physical therapy and rehabilitation treatment are tailored to the needs of each individual, but there can be significant variations among therapists and the ways they assess their patients. A single therapist might even apply different levels of force on patients at different times throughout the day.
Although force feedback is a key component of physical therapy, it typically relies on the subjective judgement of the therapist. Treatment could therefore be improved if there was a means of obtaining objective data. In fact, there are currently smart force-sensitive devices that can measure or control the amount of force applied to, or by, the patient.
Options for Embedded Force Sensing Technology
Load cells are a common type of force sensor and offer a high level of accuracy. Their large size and weight, however, are drawbacks — it is difficult to embed them into small, compact devices.
Strain gauges are another common alternative and are much smaller than load cells. Unlike load cells, though, strain gauges measure force as a result of an indirect measurement correlated to the mechanical strain of fine conductive wires. They require complex electronics that can be expensive to implement on a large scale.
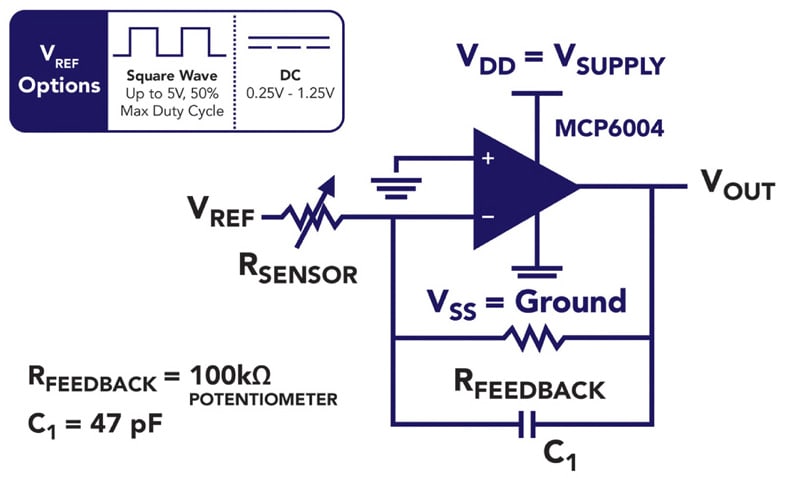
Piezoresistive touch sensors are a third alternative. They are passive elements consisting of semiconductive material sandwiched between two pieces of flexible polyester, whose resistance changes with applied force. When unloaded, the sensor has a high resistance of about 2MΩ that drops when loaded. The conductance (inverse of resistance) response of touch sensors is linear as a function of force within the sensor’s designated force range. The fact that they are passive, have linear conductance response, and a large dynamic range of resistance, allows the design engineer to use simple electronics.
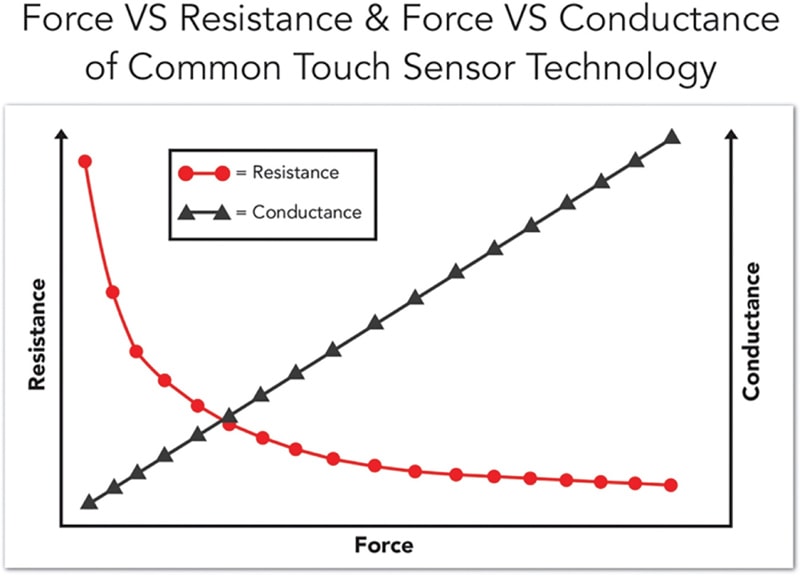
A piezoresistive sensor can be powered through an op-amp circuit or a voltage divider. With both of these circuits, the resistance change causes a corresponding change in the circuit’s output signal. This can be read by an analog-based system or digitized via an analog-to-digital converter. Depending on the setup, the force range of the sensor can be adjusted by changing the drive voltage or the resistance of the op-amp’s feedback resistor. This allows the user to have control over parameters such as maximum force range, and measurement resolution within that range.
Another benefit of the linear force-conductance relationship, is that these sensors only require simple calibration. While force-sensing applications that employ load cells or strain gauges may need to be factory calibrated after repeated use, devices based on piezoresistive touch sensors can have their calibration routine embedded into the device firmware for on-the-fly recalibration.
Physical Therapy Devices Enhanced with Piezoresistive Touch Sensors
Whether embedded into a wearable device, or onto contact points of equipment, touch sensors collect critical force data for therapists to safely and efficiently care for their patients. The following are three real-world examples of this technology in use.
Example 1. A Simple Method to Standardize Manual Evaluation Techniques
When it comes to physical therapy treatment, nothing can take the place of a hands-on manual assessment. However, using a minimally-invasive method to measure force applied to the patient can improve assessment quality and consistency.
With this in mind, researchers from the Griffith University of Queensland, Australia, developed an inexpensive, user-friendly, wearable force-sensitive device as a method to train physical therapy students on proper force application. Touch sensors attached to key contact points of the device were used to transmit real-time force readings to a computer. The researchers used simple wiring and a computer’s sound card in place of an analog-to-digital converter without additional electronic components. The card’s output signal is applied to the touch sensor, and the modified signal is returned via a microphone jack, such that the touch sensor acts as a volume control. The computer software reads the intensity of the return signal, converts the value into a force equivalent, and displays the force as both an instantaneous value and a time-series graph. The system also produces an audible sound that serves as feedback to guide the therapist as to how they should vary the applied force.
Example 2. Quantifying Patient Hand Strength, Endurance, and Agility
It is disheartening when a joint injury or nerve damage restricts a person from doing everyday activities. Unfortunately, patients diagnosed with Rheumatoid Arthritis (RA), Systemic Sclerosis (SS), and carpal tunnel syndrome, know this struggle all too well.
A group of bioengineers recently designed a low-cost gripping device consisting of touch sensors to monitor a patient’s progress through rehabilitation sessions. The device provided force feedback while the patient executed seven common hand exercises including hand pinch, grip, and isometric rotation. Sensors were positioned between two halves of a handle, and were covered with neoprene.

The grip device is interfaced with a low-power micro-control unit that includes a signal conditioning stage followed by digitization via an analog-to-digital converter. Signal conditioning consists of low-pass active filters. Since all signals coming from the touch sensors are unipolar, a single supply configuration without any biasing circuitry could be employed. This minimized circuit complexity and reduced power-line interference.
As the patient grips the device, a digitized buzzer sound indicates the minimum applied grip force needed to execute the next tasks. A computer program also maintains a log of the patient’s progress with each use of the device.
In a study involving 20 patients diagnosed with RA and SS, results showed significant improvement in the patients’ ability to make these movements with greater strength and proficiency after only 12 weeks. A similar device could also be developed for the patient to use while away from the treatment facility.
Example 3. A Tongue Exercise Tool for Neurological Recovery
After a significant neurological event such as a brain injury or stroke, patients may need to retrain their facial muscles to perform common functions like chewing or swallowing. Speech pathologists, in their own way, are physical therapists who help patients to not only regain their ability to speak, but also to strengthen their tongue and orofacial muscles.

An innovative system involving a mouth guard embedded with touch sensors — developed by an engineering group from the Universidade Federal de Minas Gerias in Brazil — measures the health of a patient’s orofacial muscles. Signal conditioning op-amps provide linearization and conversion of the electrical resistance into voltage.
The data acquisition system of the mouth guard device is composed of three main modules: an antialiasing filter, an analog-to-digital converter, and serial communication. Matlab-based software captures and generates a report presenting the force profile of the patient. The report displays graphical records of the force-over-time profiles of three different measurements made by the patient’s tongue on the mouth guard, including the maximum and average forces, and mean and standard deviations.
With this data, speech pathologists can keep a log of their patient’s progress and monitor the effectiveness of their treatment program.
Make the Path to Recovery Safer, and More Efficient
Given the important role of human contact in physical therapy, there is a natural vulnerability to human error. Force-sensitive devices that help physical therapists quantify how they interact with patients, benchmark their progress, and build confidence in their treatment methods, can be key tools to advance the future of physical therapy.
This article was written by Mark Lowe, Vice President of Sensors, Tekscan (South Boston, MA). For more information, contact him at