For many people, gastrointestinal (GI) disorders are chronic and life-altering conditions. Yet despite their prevalence, doctors are often challenged by patients experiencing persistent symptoms with no way to accurately identify and diagnose diseases.
Kennesaw State University’s Lei Shi — an assistant professor of mechanical engineering in the Southern Polytechnic College of Engineering and Engineering Technology (SPCEET), along with Dr. Anand Jain from Emory University — is working to change that. Supported by a recent National Science Foundation (NSF) grant, Shi is leading a research project that could alter how GI disorders are diagnosed and treated using virtual replicas of a human stomach.
“This research is personal for me,” Shi said. “I’ve experienced stomach issues myself, and I know how disruptive they can be. Many people feel discomfort, nausea, or digestive problems, but after an endoscopy or imaging, they’re told everything looks normal. We want to understand what’s going on at a deeper level.”
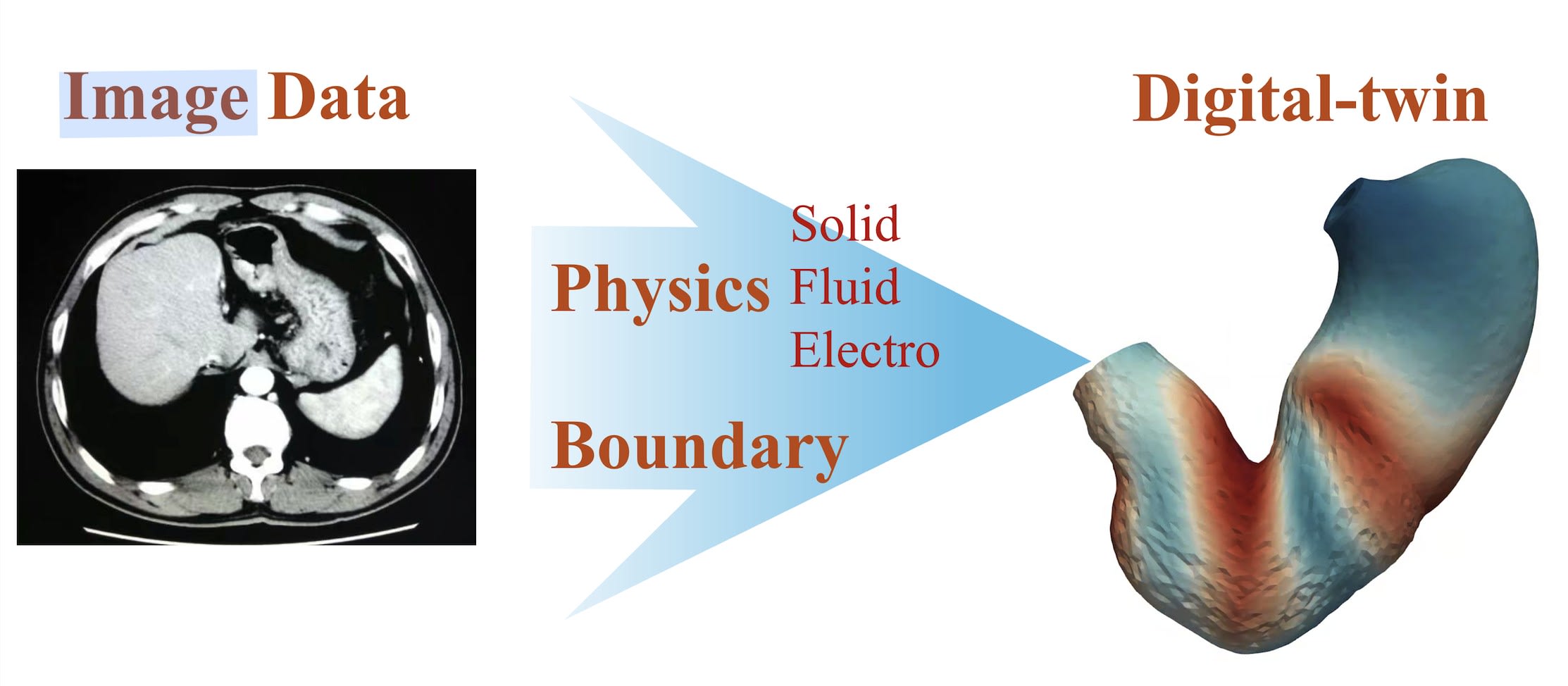
Shi’s approach is based on two key assumptions. First, microscopic changes in the stomach’s mechanical properties can exist even when the organ appears normal. Second, that disruptions in the stomach’s natural electrical signaling patterns can alter how it contracts and moves food. By combining advanced medical imaging, biomechanics testing, and computational modeling, his team is developing patient-specific “digital twins.” These twins are virtual models of a person’s stomach that simulate both its physical structure and its electrical activity.
The research involves collaboration with two physicians at Emory University, who provide Shi with data, including CT scans, endoscopy images, and a specialized measurement called manometry, which records pressure changes and deformation in the stomach and esophagus. In his Intelligent Biomechanics lab on KSU’s Marietta Campus, Shi and his team integrate this data into 3D models, then run biomechanical tests such as tensile and biaxial testing to determine the tissue’s stiffness and elasticity.
“Two stomachs may look the same, but one might be stiff while the other is soft. That difference affects how it moves,” Shi said. “By combining mechanical properties with electrical activity patterns, we can create a model that behaves just like the real organ.”
These digital twins could have far-reaching implications. Not only could they help detect subtle changes in the stomach that current tools miss, but they could also serve as a testbed for treatment planning.
“Dr. Shi’s innovative research demonstrates the power of collaboration to create a better life for all,” SPCEET Dean Lawrence Whitman said. “By merging engineering, computer science, and medicine, his work has the potential to transform both scientific understanding and patient care.”

Shi’s vision does not stop at the stomach. His goals include expanding the modeling to the entire GI tract from the esophagus to the intestines and studying its interaction with other systems, such as the brain-gut axis. He also plans to incorporate machine learning to speed up analysis and prediction. By applying lessons learned from his previous work modeling the heart, uterus, and cervix, Shi hopes to accelerate progress and develop a virtual platform for studying digestive function.
Here is an exclusive Tech Briefs interview, edited for length and clarity, with Shi.
Tech Briefs: What was the biggest technical challenge you faced while developing these patient-specific digital twins?
Shi: First, I want to succinctly explain what a digital twin is. In our case a digital twin is just a virtual copy of the organ. We start from the patient's medical images and clinical data to build up a computational model that mimics how the organs move and function. But we don't just mimic the shape here in this work; we build physical models that connect what happens at the molecular level and the cellular level all the way up to the whole organ and eventually to patient populations.
We can use this kind of model to serve as a virtual test bed for virtual surgery and virtual treatment planning for the organ. For example, if we cut this a little bit and we make this part a little bit stiffer, what will happen, and can we restore the normal function of the heart?
Actually, it is very similar to how engineers test airplanes in simulations before flying. Digital twins are already the gold standard in some industries. We want to bring the same idea into medicine.
So, with regards to the biggest technical challenges, there were several here. Unlike the airplane example I just mentioned, no two patients are alike. Everybody’s organs are different, which makes patient modeling much more challenging than other industries. So, the biggest hurdle was balancing the biological complexity with computational efficiency.
Tech Briefs: Do you have any set plans or further research, work, etc.?
Shi: Yes. We are expanding from the stomach to the entire upper GI tract.
From the physical esophagus, for example, through the intestine. We will explore how it interacts with the brain-gut axis. We know that the brain is influenced by the gut and intestines.
Another step is integrating advanced AI methodology, such as generative models and neural networks to make the predictions faster and more personalized.
I also want to express my appreciation to the National Science Foundation, who supports fundamental research like this.
And we are working with the clinicians to validate these models against real patient data. This is the important next step, which is very necessary for translating this into the health care practice.
My long-term goal is actually simple but important. I think it works for everybody. I want to help people feel healthier and happier when they eat and drink.
Tech Briefs: Those are all the questions I have. Is there anything else you'd like to add that I didn't touch upon?
Shi: One exciting aspect is that these digital twins aren't just a tool for doctors; they can automatically empower patients. Imagine having your own personalized model that helps predict how your body might respond to a treatment or even to a change of diet. That is powerful.